Projects
Treatment of hepatitis B in Ethiopia: a pilot program

Hepatitis B kills more than a million people worldwide each year. A simple tablet treatment exists but is unavailable to most people living in Africa.
In 2015, EtNoHep established a treatment program for 1300 patients living with chronic hepatitis B at St. Paul’s Hospital in Addis Ababa. This cohort has been followed up closely since 2015 and approximately 300 have started antiviral therapy. The study participants are well characterized with viral markers, liver enzymes and liver stiffness measurements, and this cohort is a unique source of knowledge about the natural course and treatment effect of hepatitis B in Ethiopia.
Unexplained liver disease in eastern Ethiopia
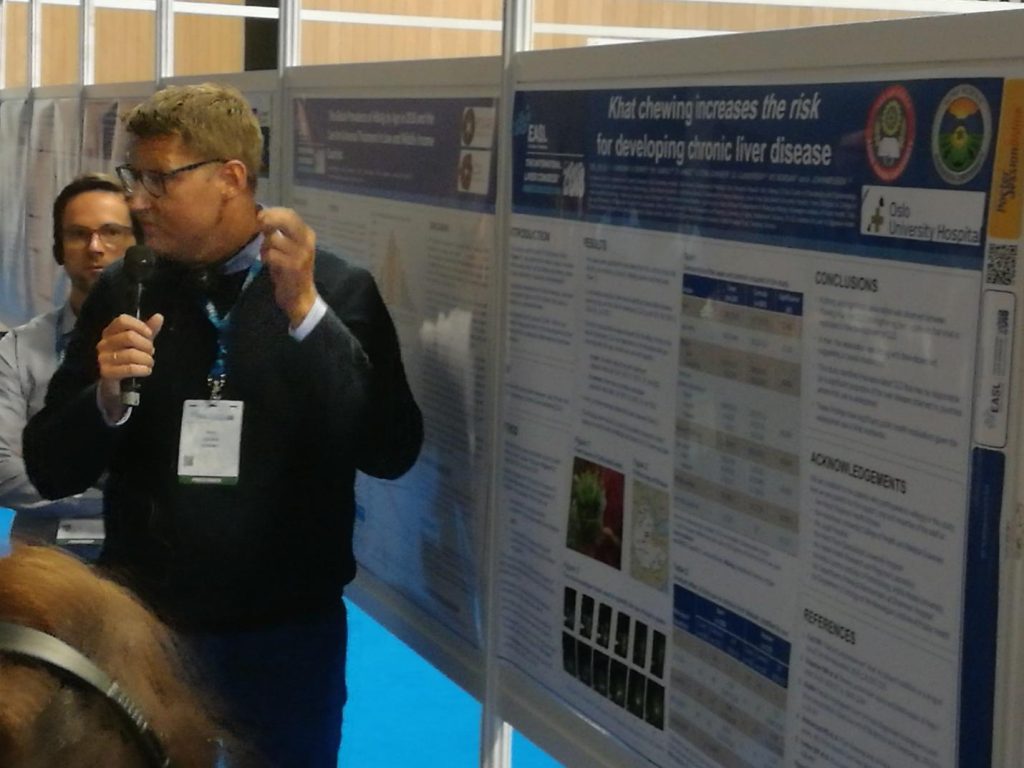
Our collaborators in eastern Ethiopia reported a high prevalence of unexplained liver disease in 2014. We set up a case-control study to try to find the underlying causes. Over a period of one year we included 150 cases with overt liver disease and 300 healthy controls from public hospitals in Harar. All patients were examined with state-of-the-art methods to assess for infectious, autoimmune and metabolic liver diseases, but even after a thorough examination more than half of the patients still had no explanation.
However, we found a strong association between chewing of khat and the development of overt liver disease among men in the study. The study was published in the acclaimed journal Hepatology.
Scale-up program for chronic hepatitis B

In the pilot program in the capital Addis Ababa we showed how hepatitis B treatment can be established and sustained in a low-income country. However, to improve the impact it is imperative to take hepatitis B treatment out to the regional hospitals.
In the scale-up program we aim to further simplify and operationalize CHB treatment in Ethiopia. We have developed and implemented a simplified treatment guideline appropriate for scaling up to a larger patient population. Since December 2021, we have enrolled 6,000 patients with chronic hepatitis B in four selected district hospitals in Adama, Jimma, Jigjiga and Semera. The aim of this project is to assess the efficacy and fasibility of a simplified protocol for hepatitis B care.
Decentralized hepatitis B care in Ethiopia
With this new undertaking to be started in September 2024, we aim to decentralize CHB therapy to rural settings, which will be essential to achieve universal access to antiviral therapy in Africa. We will study different treatment models, each of which has its theoretical pros and cons:
i) standard model (‘treat only if …”),
ii) inclusive model (“treat all except…”),
iii) test-and-treat (“treat alt’).
The primary endpoint will be death or liver decompensation, and secondary endpoints will be programmatic and laboratory success indicators. Finally, we will compare the cost-effectiveness of these decentralized models with the central hospital-based model.
Implementation research, such as our study, is of vital importance to respond to the research gaps identified by the World Health Organization in hepatitis B care. Our study is expected to directly inform international hepatitis B guidelines and will be a major contribution to the efforts to eliminate viral hepatitis as a public health threat by 2030.
HEPSANET: regional collaboration in Africa
Little is known about the natural history of HBV infection, determinants of disease progression, and response to antiviral therapy in African CHB patients. Most of our knowledge about HBV comes from Asia, but this can not be extrapolated to Africa because of differences in circulating HBV genotypes, co-infections, co-morbidity and environmental exposures. As an example, HCC may occur at a younger age in SSA compared to other regions, suggesting that other risk factors may be involved.
HEPSANET (Hepatitis B in Africa collaborative network, www.hepsanet.org) was established to create a de-identified registry for chronic hepatitis B in Africa. Our aim is to establish a longitudinal registry of CHB patient in SSA, which can answer current and future clinical and public health questions. EtNoHep is one of the founding members of HEPSANET.
Effectiveness of timely hepatitis B birth dose vaccination in Ethiopia
Hepatitis B vaccination is the cornerstone of global initiatives to eliminate hepatitis B. Historically, mother-to-child transmission (MTCT) of HBV was considered uncommon in Africa, leading to a reluctant attitude to birth-dose HBV vaccination on the continent. However, 2 of 3 new HBV infections now occur in Africa, translating into 990,000 new HBV infections annually.
In Ethiopia, birth-dose HBV vaccination is not part of the National policy, but some centres have offered this as part of a MoH pilot program. In a Gavi supported study we will assess the rate of MTCT of HBV in centres with and without birth-dose HBV vaccination, and thereby the effectiveness of the birth dose vaccine in a real-world setting.
